Bacterial vaginosis
Notes
Overview
Bacterial vaginosis refers to an overgrowth of predominantly anaerobic microorganisms in the vaginal flora.
Bacterial vaginosis (BV) refers to a condition where there is disruption in the normal vaginal flora. There is an excess of anaerobic microorganisms and loss of the normal lactobacilli, which leads to a vaginal odour and increased discharge.
The condition is a not a sexually transmitted infection (STI) but it occurs more commonly in sexually-active women.
Epidemiology
BV is the most common cause of vaginal discharge in women of childbearing age.
Almost one third of women between the ages of 14-49 years old have evidence of BV. It is highest amongst women who are sexually active.
BV is seen more commonly in black women. Women who have sex with women are more at risk due to shared vaginal flora patterns.
Aetiology & pathophysiology
BV occurs due to a loss of the usual lactobacilli bacteria within the vaginal flora.
The exact trigger for BV is unknown. However, a rise in the vaginal flora pH >4.5 creates an alkaline environment that favours colonisation by anaerobic organisms, such as Garnerella vaginalis and loss of the usually dominant lactobacilli.
Example of organisms found in BV:
- Gardnerella vaginalis
- Prevotella species
- Bacteroides species
- Peptostreptococcus species
It is the alteration in the relationship between G. vaginalis, other organisms and Lactobacilli that leads to the development of BV. This is often described as a synergistic polymicrobic infection.
The absence of inflammation BV is why the term vaginosis is preferred to ‘vaginitis’, which implies inflammation.
Risk factors
- Sexual contact: sexual activity, change in sexual partner, women who have sex with women, semen in vagina, oral sex
- Hygiene: use of vaginal hygiene products (e.g. douches, deodorant, and vaginal washes)
- Other: menstruration, black women, copper coil, smoking
Clinical features
The presence of a vaginal odour is the most common presenting symptom.
Symptoms
- Asymptomatic (50%)
- Vaginal odour: may only be noticed after sexual intercourse (semen is alkaline, which causes amines to be released that gives a fishy odour)
- Vaginal discharge: typically thin, off-white/grey and homogeneous
- Irritation of vulva (uncommon)
- Dysuria (rare)
- Dyspareunia (rare)
Signs
- Vaginal discharge: thin, off-white/grey and homogenous. May adhere tightly to vaginal mucosa.
- Normal speculum: apart from discharge, the rest of the examination is usually normal. Any lesion or cervicitis warrants further investigation
Diagnosis
The diagnosis of BV is based on the Amsel criteria.
The diagnosis of BV can be made when three of the four Amsel criteria are met:
- Vaginal pH > 4.5
- Typical discharge: thin, off-white/grey, homogenous and smoothly coats vaginal wall
- Positive whiff-amine test: development of fishy odour with addition of 10% potassium hydroxide to vaginal discharge
- Clue cells (on microscopy): vaginal epithelial cells studded with adherent coccobacilli
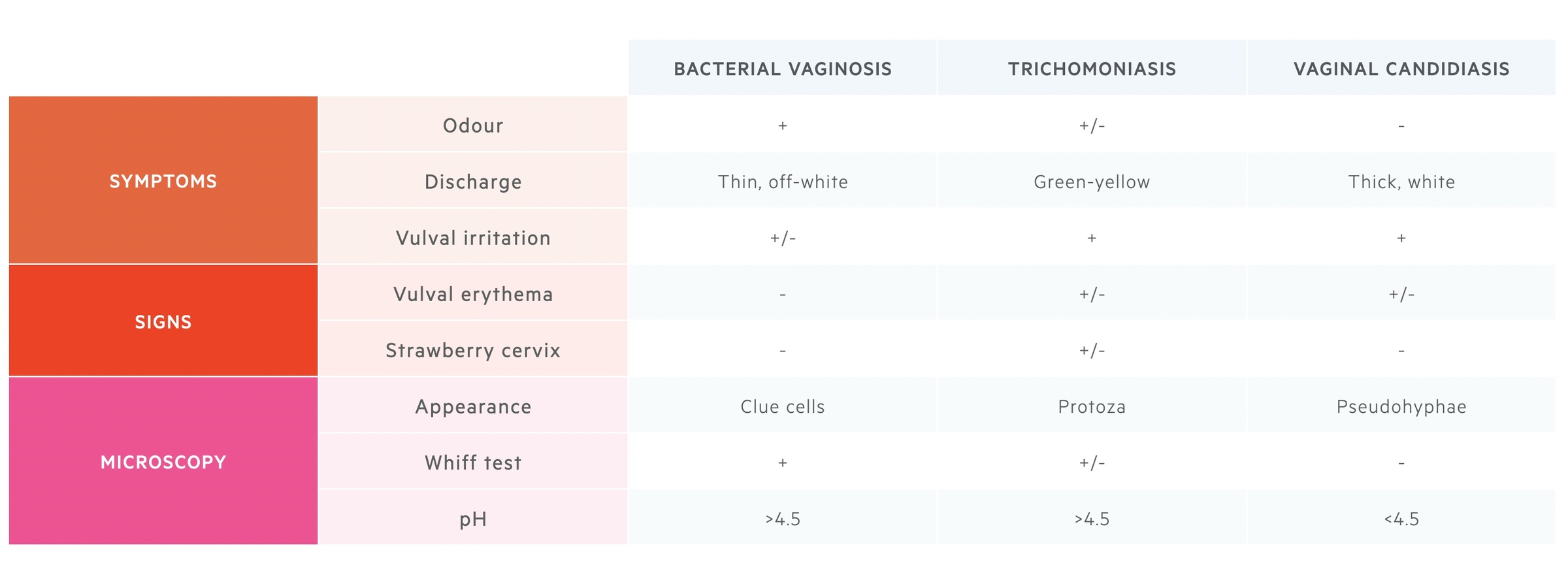
Differential diagnosis
Other conditions such as trichomoniasis and candidiasis may present similarly to BV. These conditions are usually associated with soreness, itching or irritation. Remember there could be co-infection and samples are usually required to differentiate between these pathologies.
Investigations
Investigations are needed for a formal diagnosis of BV.
Formal examination of the vulva with speculum examination is needed to make a diagnosis of BV. However, patients who fulfil certain criteria with features that are highly specific for BV may be treated empirically.
Bedside
- Vulval examination (external female genitalia): assess for lesions, discharge, ulcers and inflammation
- Speculum examination: visualise the cervix and vaginal walls. Take high vaginal swabs.
Vaginal discharge testing
Samples should be taken from the lateral wall and then tested for pH using a low-range pH paper. Normal vaginal pH in women of child-bearing age is 3.5-4.5. Samples with pH > 4.5 is suggestive of BV.
Samples can also be checked for Clue cells by using microscopy. Clue cells refer to vaginal epithelial cells that have many coccobacilli adherent to their surface, giving a studded appearance and less sharply defined border.
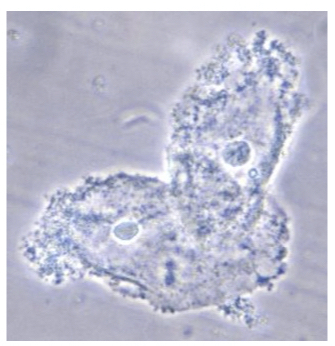
Evidence of Clue cells under light microscopy. Image courtesy of CDC.
Microbiology
- High vaginal swabs: taken for gram stain and to rule out other causes (e.g. STI testing). Gram stain is the gold-standard but rarely used in clinical practice.
STI screen
Consider testing for the following STIs and referring as necessary to a genito-urinary medicine (GUM) clinic among high-risk patients.
- Chlamydia
- Gonorrhoea
- Trichomoniasis
- HIV/syphilis: may be required depending on the indication and high-risk sexual behaviour.
Management
Oral metronidazole is the treatment of choice in symptomatic patients.
Empirical treatment
Patients may be given empirical treatment based on the history if there is a low risk of STI and none of the following factors are present:
- No previous gynaecological procedure
- Not associated with miscarriage or termination of pregnancy
- No other explanation for discharge
- First episode
Recurrent episodes may be treated empirically if they have been previously confirmed following examination.
Standard treatment
Women who are asymptomatic do not require treatment unless they are undergoing termination of pregnancy. The treatment of women who are symptomatic depends on pregnancy status. In general, metronidazole orally or as a pessary may be given to non-pregnant patients and in pregnant patients metronidazole may be given but it should be discussed with the patients' obstetrician.
NOTE: Clindamycin can be used as an alternative as both an oral and intravaginal preparation.
In patients with persistent or recurrent BV, an assessment of adherence, a full speculum examination, and high vaginal swabs are critical. Prolonged courses may be given for persistent BV but additional advice should be sought from a sexual health or gynaecology clinic. If associated with an IUD, this should be removed. A recurrent episode may be treated again with a longer course of metronidazole and prophylactic intravaginal treatment can be considered for ≥4 episodes but this is off-label.
Complications
BV is associated with an increased risk of post-surgical infections (e.g. post-C-Section).
BV increases the risk of salpingitis, endometritis, and infections following surgery (e.g. post-hysterectomy, post-cesarean). It can also increase the risk of pregnancy complications.
Last updated: October 2024
Have comments about these notes? Leave us feedback
