Hyponatraemia
Notes
Definition & classification
Hyponatraemia is a common medical problem defined as a low plasma sodium (Na+) concentration less than 135 mmol/L.
The normal range for serum sodium is 135-145 mmol/L. Hyponatraemia can be classified according to the severity of the biochemical value or the rate of onset.
Biochemical severity
- Mild hyponatraemia: serum Na+ 130-135 mmol/L.
- Moderate hyponatraemia: serum Na+ 125-129 mmol/L.
- Severe hyponatraemia: serum Na+ < 125 mmol/L.
Rate of onset
- Acute: duration < 48 hours.
- Chronic: duration > 48 hours
Epidemiology
Hyponatraemia is a common electrolyte disturbance encountered in primary and secondary care.
The incidence and prevalence of hyponatraemia is variable and dependent on the population studied. Some studies indicate that it is the most common electrolyte abnormality seen in clinical practice.
Physiology
The concentration of serum sodium is determined by the total body water.
Sodium is one of the main determinants of effective osmolality within the extracellular fluid. Osmolality is the concentration of a solute dissolved in a solution. Effective osmolality or ‘tonicity’ is essentially the effective osmotic pressure gradient.
In other words, tonicity governs the transcellular distribution of water. Normal plasma osmolality is approximately 275-295 mOsm/L. It can be estimated using the formula 2Na + urea + glucose. Antidiuretic hormone (ADH) is the key hormone involved in osmoregulation
ADH is produced by the magnocellular neurons in the paraventricular and supraoptic nuclei of the hypothalamus. It is stored and released by the posterior pituitary in response to rising plasma osmolality. It may also be referred to as arginine vasopressin (AVP) or simply vasopressin.
ADH release begins at a plasma osmolality of around 280 mOsm/kg. Thirst is felt at around 290 mOsm/kg. These processes lead to a reduction in the plasma osmolality.
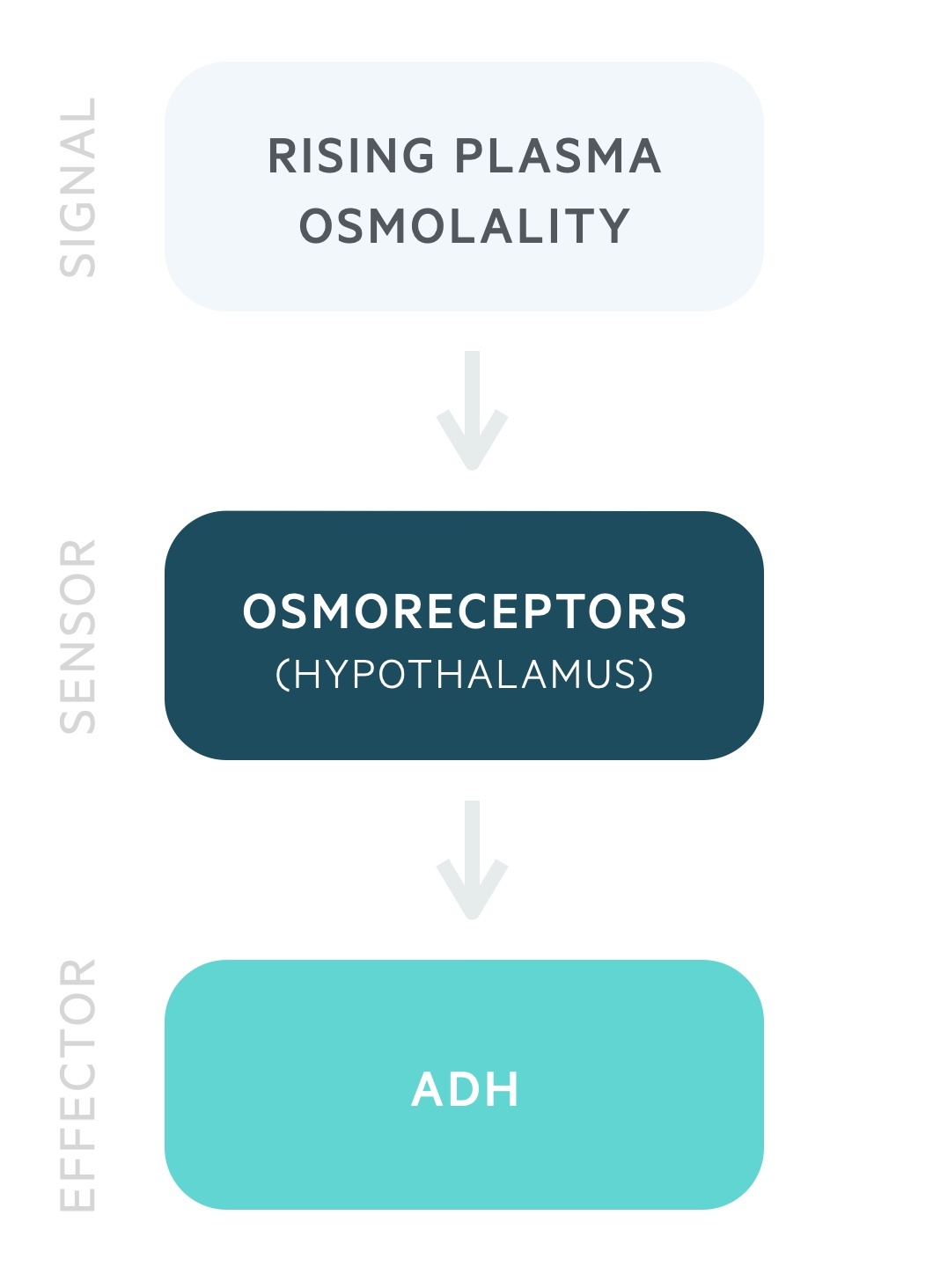
ADH acts on the distal convoluted tubule and collecting duct to increase water reabsorption independent of sodium. ADH stimulates the insertion of aquaporin-2 channels onto the luminal membrane, allowing the free entry of water. ADH also causes vasoconstriction of arterioles.
Aetiology
There are an numerous causes of hyponatraemia and multiple mechanisms may contribute.
The aetiology of hyponatraemia can be broadly divided into three categories based on fluid status: hypovolaemia, euvolaemia, hypervolaemia.
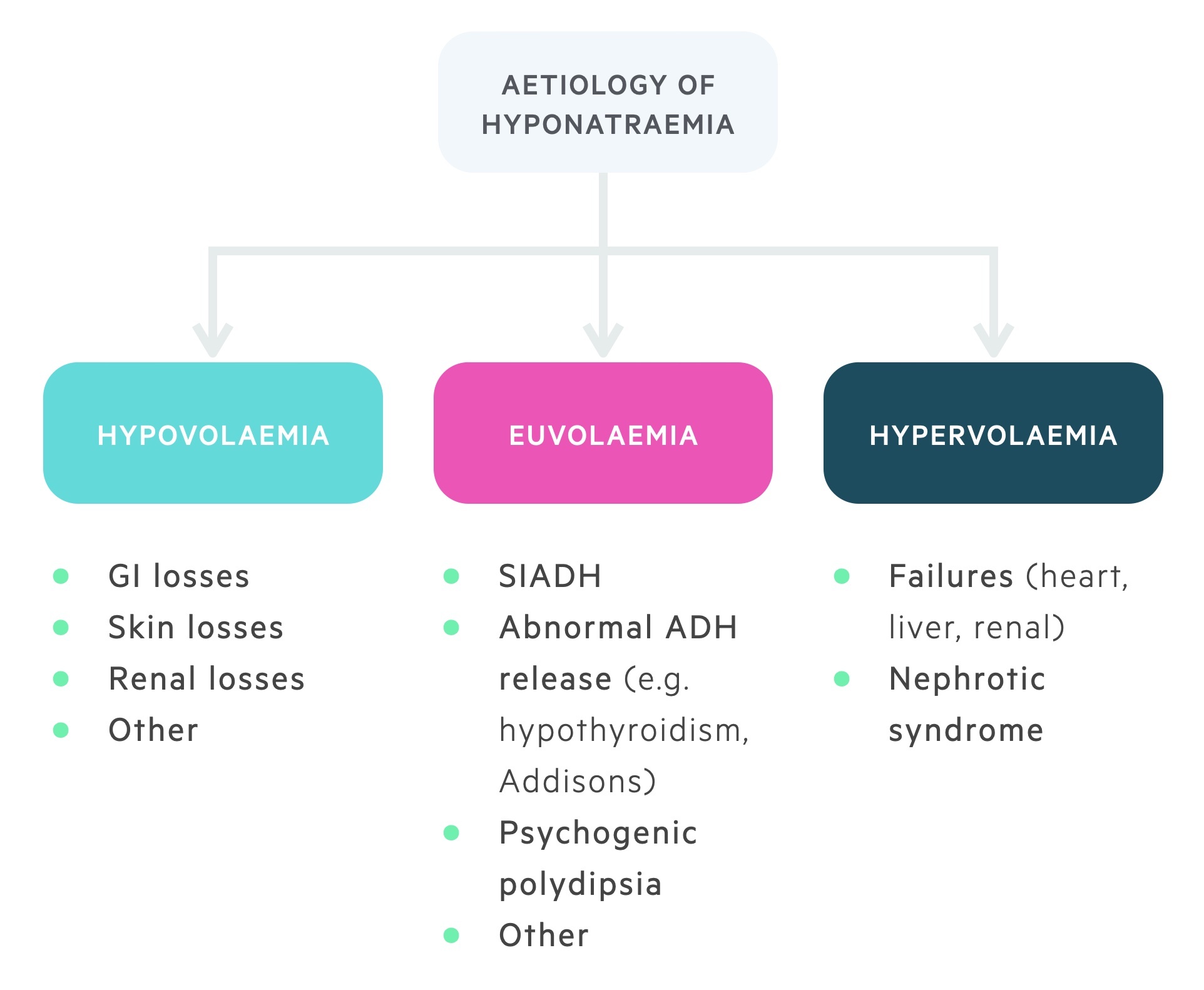
Hypovolaemia
Hypovolaemia refers to a reduction in extracellular fluid status. If there is a greater loss of sodium relative to total body water then hyponatraemia will ensue.
The three most common categories of hypovolaemic hyponatraemia are gastrointestinal losses, skin losses and renal losses.
- Gastrointestinal losses
- Severe diarrhoea and/or vomiting
- Pancreatitis
- Skin losses
- Sweating
- Burns
- Renal losses
- Medications (e.g. diuretics)
- Salt-wasting nephropathies
- Other
- Primary adrenal insufficiency (i.e. Addison's disease)
- Sepsis (third space losses)
- Cerebral salt-wasting
Euvolaemia
Euvolaemia refers to a normal extracellular fluid status. The main cause of euvolaemic hyponatraemia is SIADH.
The causes of euvolaemic hyponatraemia include:
- SIADH
- Hypothyroidism
- High water, low solute intake (i.e. primary polydipsia, anorexia nervosa)
Hypervolaemia
Hypervolaemia refers to an increase in extracellular fluid status. If there is an increase in total body water relative to sodium then hyponatraemia will ensure.
The main causes of hypervolaemic hyponatraemia are the ‘failures’ and nephrotic syndrome.
Pseudo-hyponatraemia
False hyponatraemia can occur as an artefactual result due to a significant rise in serum proteins or serum lipids. This is termed pseudohyponatraemia.
Fluid status assessment
The assessment of fluid status is critical to determine the underlying cause of hyponatraemia.
Assessment of fluid status is done clinically at the bedside. It involves looking for features that are suggestive of dehydration (i.e. hypovolaemia) or features suggestive of overload (i.e. hypervolaemia). If neither are present then the patient may be considered clinically euvolaemic.
Hypovolaemia
- Dry mucous membranes
- Capillary refill time > 2 seconds
- Dizziness
- Thirst
- Postural drop in systolic blood pressure
- Tachycardia
Hypervolaemia
- Raised JVP
- Bibasal crackles
- Gallop rhythm
- Peripheral oedema
- Hypertensive
Clinical features
Hyponatraemia is often asymptomatic, where symptoms are present they are usually vague and non-specific.
- Headache
- Confusion
- Nausea and vomiting
- Lethargy
- Irritability
- Seizures
- Loss of consciousness
- Coma
Clinical features may also reflect the underlying aetiology (e.g. shortness of breath in heart failure, abdominal pain in pancreatitis).
Clinical severity
- Mild: asymptomatic or mild features of nausea, lethargy, irritability
- Moderately severe: nausea, confusion, headache
- Severe: vomiting, cardiorespiratory distress, abnormal and deep somnolence, seizures, coma
Diagnosis & investigations
Hyponatraemia is diagnosed based on the finding of a low serum sodium concentration on blood testing.
The diagnosis in the majority of cases of hyponatraemia is incidental during routine blood tests.
Investigating the cause of hyponatraemia is largely dependent on the suspected underlying cause. Key investigations can be divided into blood tests and urinary tests.
Urinary tests
- Urinary osmolality
- Urinary sodium
Blood tests
- U&E
- Glucose
- Lipids
- Thyroid function tests (TFTs)
- Liver function test (LFTs)
- Early morning cortisol
A paired urine and plasma osmolality are important in determining the cause of euvolaemic hyponatraemia. In SIADH, the plasma osmolality is typically low (i.e. < 275 mOsm/kg), urine osmolality high due to an inability to dilute urine (i.e. > 100 mOsm/kg) and the urinary sodium is high (> 30 mmol/L). However, it is important to remember that SIADH is diagnosis of exclusion.
Acute hyponatraemia
The management of acute hyponatraemia largely depends on the presence or absence of neurological symptoms.
Patients with acute hyponatraemia should be managed in a high-dependency unit (HDU), especially if neurological symptoms are present, and have their sodium levels checked regularly.
Mild or absent neurological symptoms
Management should be directed at the underlying cause. Medications should be reviewed to identify possible causes of hyponatraemia and non-essential parental fluids should be stopped.
Moderate or severe neurological symptoms
Patients require rapid correction of serum sodium concentration to reduce the risk of complications with the use of hypertonic saline (i.e. 1.8-3% sodium chloride).
Chronic hyponatraemia
The management of chronic hyponatraemia is based upon the underlying aetiology.
It is important to avoid overly aggressive normalisation of sodium levels, correction should never exceed 8-10 mmol/L per 24 hours. More rapid corrections risk the development of osmotic demyelination syndrome.
Hypovolaemic
Patients who are fluid deplete require intravenous replacement with normal saline. As fluid is given, there should be a correction in the serum sodium concentration.
A medication review should also be completed to identify any drugs contributing to or directly causing hyponatraemia (e.g. diuretics, SSRIs).
Euvolaemic
The most common cause of euvolaemic hyponatraemia is SIADH. Therefore, patients are usually managed with fluid restriction in accordance with SIADH management unless another cause is identified.
Patients with SIADH may require medical treatment to prevent the action of ADH on the distal coveted tubules. Options include demeclocycline or Vaptans (e.g. tolvaptan). Demeclocycline works as an inhibitor of ADH and the Vaptons act as a vasopressin receptor antagonist. If no clear cause is identified on initial investigations then patients should be investigated for underlying malignancy.
Hypervolaemic
Patients with hypervolaemic hyponatraemia require treatment of the underlying cause.
As a general rule, these patients are managed with fluid and salt restriction and the use of diuretics, especially in heart failure. As the fluid is off-loaded from the body, there should be an improvement in sodium levels.
Complications
Hyponatraemia is a potentially life-threatening condition, especially with a rapid decline in sodium levels, or levels that fall < 120 mmol/L.
Cerebral oedema
Hyponatraemia can result in large fluid shifts due to changes in osmolality. The most significant of this is fluid shifts into cells of the central nervous system leading to cerebral oedema. Cerebral oedema causes raised intra-cranial pressure, which can lead to altered mental status, seizures, coma and death.
If hyponatraemia is more chronic, it can predispose to issues with falls, gait disturbance, concentration problems and cognitive deficits.
Osmotic demyelination syndrome
Also termed cerebral pontine myelinolysis, osmotic demyelination syndrome is caused by rapid correction of hyponatraemia. Such correction can lead to large shifts of intracellular water affecting the pons and other parts of the central nervous system. This can then precipitate irreversible neurological damage, which usually occurs 2-4 days following the rapid correction.
Osmotic demyelination syndrome typically results in the development of quadriplegia and pseudo-bulbar palsy although other neurological features can occur. To prevent this complication, in absence of severe neurological features from hyponatraemia that might require more rapid correction, sodium correction should not exceed 8-10 mmol/L per 24 hours.
Last updated: October 2024
Have comments about these notes? Leave us feedback
