Horner's syndrome
Notes
Overview
Horner’s syndrome refers to a classic triad of miosis, ptosis and anhidrosis.
Horner’s syndrome is a classic medical condition that is characterised by a unilateral triad of:
- Miosis: small pupil
- Ptosis: drooping eyelid
- Anhidrosis: lack of sweat
Horner’s syndrome is due to a lesion anywhere along the sympathetic pathway, also known as the oculosympathetic pathway. This pathway is important for pupillary dilatation. As such, Horner’s is also known as oculosympathetic paresis.
Pupillary response
The sympathetic nervous system has an important role in pupillary dilatation.
Both the sympathetic and parasympathetic nervous systems are involved in pupillary responses. This helps to control how much light is reaching the retina.
- Parasympathetic pathway (constricts): mediated by the oculomotor and optic nerves as part of the pupillary light reflex.
- Sympathetic pathway (dilates): mediated via first, second and third order neurons.
The sympathetic nervous system forms the oculosympathetic pathway. Activation of this pathway may occur when there is too little light for normal retinal function or as part of the ‘fight-or-flight’ response. Activation causes pupillary dilatation through contraction of the radial fibres of the iris (i.e. pupillary dilator).
Oculosympathetic pathway
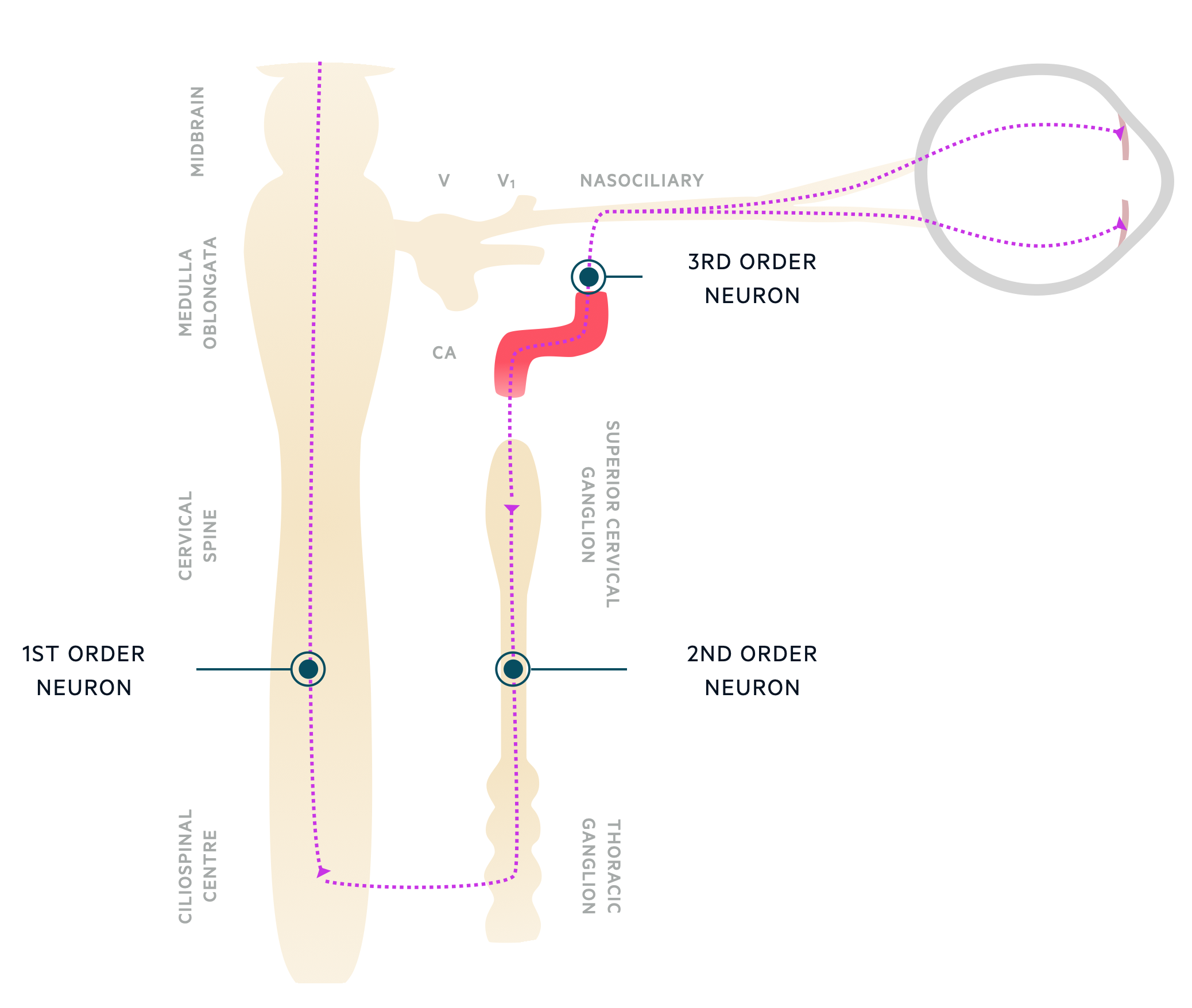
The oculosympathetic pathway is composed of three neurons: first, second and third order.
Knowledge of the neuroanatomy of the oculosympathetic pathway is important because it helps us determine the possible aetiology. Horner’s syndrome can develop due to a lesion anywhere along this pathway.
First-order neuron
Known as the central neuron. Fibres travel from the hypothalamus to the spinal cord (C8-T2). This area of the spinal cord is known as the ciliospinal centre of Budge.
Second-order neuron
Known as the pre-ganglionic neuron. Its fibres exit the spinal cord via the dorsal roots and enter the sympathetic chain. Here they travel upwards over the apex of the lung to the superior cervical ganglion.
Third-order neuron
Known as the post-ganglionic neuron. Its fibres pass within the adventitia of the internal carotid artery. They join the ophthalmic portion of the trigeminal nerve at the cavernous sinus and subsequently pass to the pupillary dilator via ciliary nerves.
The post-ganglionic sympathetic fibres also innervates a small muscle known as ‘Müller's muscle’. This muscle contributes a small proportion to upper eye lid elevation and lower lid retraction. This is why ptosis is a phenomenon of Horner’s.
Aetiology & pathophysiology
Horner’s syndrome develops due to a lesion anywhere along the oculosympathetic pathway.
The aetiology of Horner’s syndrome can be divided by the order of neuron affected.
First order
Caused by a lesion anywhere between the brainstem and cervicothoracic spinal cord. Lesions of the central nervous system are usually present with other neurological features.
- Stroke (e.g. lateral medullary syndrome): most common cause of first-order lesion. Other features of lateral medullary syndrome include vertigo, nystagmus, ataxia (ipsilateral), pain and temperature loss (contralateral body, ipsilateral face), nausea/vomiting, dysphagia, and hiccups.
- Space-occupying lesion
- Multiple sclerosis
- Syringomyelia (fluid-filled cyst spinal cord)
- Cervical cord trauma
Second order
The classic cause of Horner’s syndrome affecting the second-order neuron is a pancoast tumour. This refers to a tumour in the apex of the lung.
- Pancoast tumour
- Thoracic outlet lesion
- Trauma (e.g. brachial plexus injury)
- Thoracic aneurysm
Third order
The most concerning cause of Horner’s secondary to a third-order neuron lesion is carotid artery dissection. The should be suspected in any patient presenting with an acute, painful Horner’s syndrome. Up to 60% of carotid artery dissection will have an isolated, ipsilateral Horner’s syndrome on presentation.
- Carotid artery dissection
- Carvernous sinus pathology (e.g. aneurysm, thrombosis)
- Neck mass
Clinical features
Horner’s syndrome causes a classic triad of ipsilateral miosis, ptosis and anhidrosis.
Miosis and ptosis are universal to all causes of Horner’s syndrome. The degree of anhidrosis depends on which neuron has been affected. Remember, a variety of other neurological features may be present depending on the cause.
Miosis
The degree of anisocoria, which describes unequal pupils, is more marked in the dark. The pupil will also dilate slower following removal of a light source compared to the other eye.
Ptosis
Ptosis is usually minimal (<2 mm), which reflects the minimal contribution of Müller's muscle to lid elevation.
Anhidrosis
The degree of anhidrosis, which describes a lack of sweating, is dependent on the neuron affected.
- First order: affecting the ipsilateral body
- Second order: affecting the ipsilateral face. However, usually mild and only affecting the forehead.
- Third order: absent
The symptom is absent in third order lesions because the sympathetic fibres involved in facial sweating branch off at the superior cervical ganglion and follow the course of the external carotid artery.
Associated neurological features
- Brainstem signs: diplopia, vertigo, ataxia, focal weakness
- Spinal cord signs: bilateral or ipsilateral weakness, sensory level, bowel and bladder impairment
- Axillary or lung apex involvement: arm pain and/or hand weakness
- Isolated Horner’s: concerning for carotid dissection
Diagnosis & investigations
Horner’s syndrome is a clinical diagnosis that should prompt evaluation for an underlying cause.
Once identified clinically, Horner’s syndrome should warrant a search for an underlying cause such as carotid dissection or pancoast tumour. This usually requires immediate assessment and investigation.
In patients presenting with an acute Horner’s syndrome, it is pertinent to exclude a carotid artery dissection with a CT angiography due to the high risk of subsequent stroke. Those with brainstem features or symptoms localising to the cavernous sinus (e.g. multiple cranial nerve palsies - III, IV, V1, VI) warrant further investigation with MRI. An MRI spine is usually needed for suspected spinal cord lesions and a CT chest should be undertaken in suspected pancoast tumour.
Confirmation & localisation
Pharmacological tests are available to confirm Horner’s syndrome and to localise the lesion.
Confirmation
Horner’s syndrome is usually determined based on clinical assessment. However, in subtle cases, cocaine or apraclonidine drops can be used to confirm the diagnosis.
- Cocaine drops: blocks reuptake of noradrenaline at the nerve synapse. Leads to activation of the pupillary dilator and subsequent dilatation. Has no effect in eyes with impaired sympathetic innervation. Degree of anisocoria is measured after 1 hour.
- Apraclonidine: alpha agonist with weak action on alpha-1-receptors and strong action on alpha-2-receptors. Activation of alpha-1 causes pupil dilatation and alpha-2 causes pupil constriction. If administered to a ‘normal pupil' it will constrict slightly due to the stronger alpha-2 action. If administered to a ‘Horner’s pupil’ it will dilate due to alpha-1 receptor denervation supersensitivity (i.e. it’s more sensitive to the drug affects due to a period of not being stimulated).
Localisation
Hydroxyamphetamine eye drops are used to help localise the lesion to the first, second or third order neuron. Hydroxyamphetamine stimulates release of stored noradrenaline from post-ganglionic neurons. This enables it to differentiate between first or second order lesions and third order lesions.
After administration, a ‘normal pupil’, first-order lesion or second-order lesion will all result in pupillary dilatation. There is no effect on the pupil in third order lesions. Thus, it is useful for diagnosis of a post-ganglionic (i.e. third order) lesion.
Management
The treatment of Horner’s syndrome is directed towards the underlying cause.
It is most important to remember that an acute, painful Horner’s syndrome is a neurological emergency that requires urgent assessment for a carotid dissection. These patients need urgent neuroimaging and discussion with a hyperacute stroke unit (HASU). If clinical features of stroke are already present they usually require urgent transfer to the hyperacute stroke unit.
If dissection has led to stroke, these patients may be suitable for thrombolysis or mechanical therapies if they meet eligibility criteria. This should be decided by a stroke specialist in a stroke centre. In the absence of acute stroke, patients may be treated with anti-platelets or anticoagulation depending on the vessels involved (e.g. intracranial versus extracranial).
Last updated: July 2021
Have comments about these notes? Leave us feedback
