Statins
Notes
Introduction
Statins have revolutionised the management of hypercholesterolaemia.
Statins have become essential in the management of patients with, or at risk, of cardiovascular disease including coronary artery disease (CAD), cerebrovascular disease and peripheral vascular disease (PVD).
Indications
Statins were primarily created to treat hypercholesterolaemia, which is an independent risk factor for cardiovascular disease.
Statins are indicated in both primary and secondary prevention of cardiovascular disease for many conditions.
Primary prevention
- Cardiovascular risk assessment score ≥10%* and ≤ 84 years old (risk/benefit if >84)
- Cardiovascular risk assessment score ≥10%* and type 2 diabetes mellitus (T2DM)
- Type 1 diabetes mellitus (T1DM) and additional criteria (age, kidney disease, duration)
- Chronic kidney disease (CKD)
- Familial hypercholesterolaemia
*calculated using QRISK® score
Secondary prevention
Any patient with established cardiovascular disease
- Myocardial infarction
- Angina
- Stroke or transient ischaemia attack (note caution below)
- Peripheral arterial disease
Mechanism of action
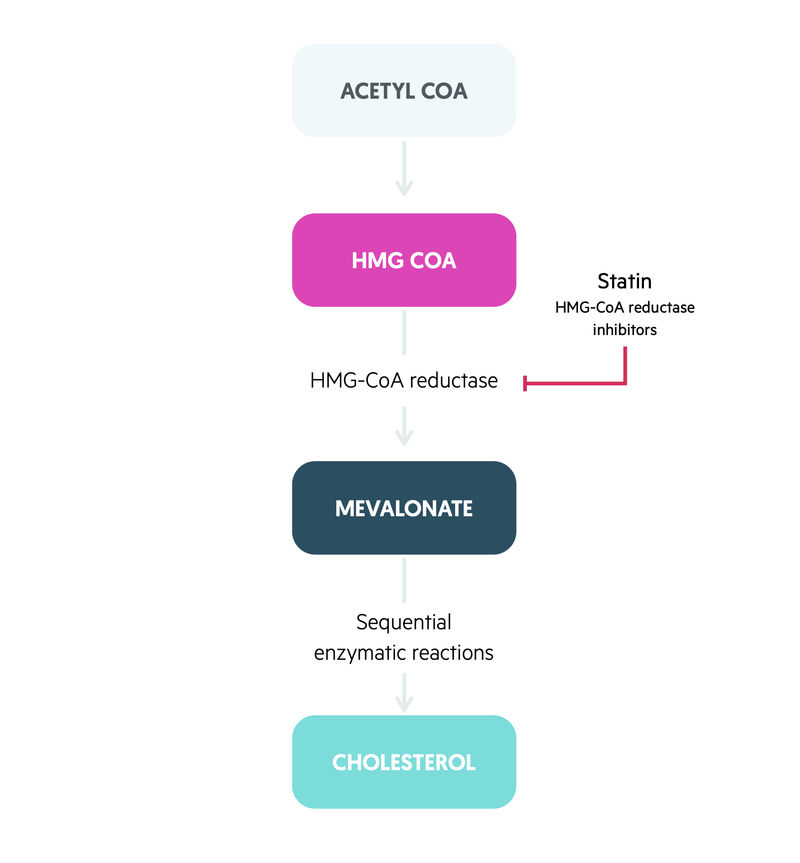
The principle mechanism of statins is inhibition of 3-hydroxy-3-methylglutaryl- coenzyme A (HMG-CoA) reductase.
HMG-CoA is an enzyme found in hepatocytes of the liver. It converts HMG-CoA into mevalonic acid, which is a cholesterol precursor. The reduction in hepatic cholesterol production leads to upregulation of hepatic LDL receptors that reduces circulating levels of LDL from the blood. The enzyme is most active at night leading to the nocturnal administration of statins.
In addition, statins have other complex cholesterol-independent effects. Statins can improve endothelial function, alter vascular smooth muscle proliferation, regulate cardiac hypertrophy, protect against ischaemic injury and exert anti-inflammatory properties. These cholesterol-independent effects support the targeted use of statins even with normal cholesterol levels.
Dosing
In the UK, the most well recognised statins available for clinical use include simvastatin, atorvastatin, rouvastatin and pravastatin.
Atorvastatin is typically started at 10-20 mg daily for primary prevention. This can be increased if necessary (every four weeks) to a max of 80 mg (for example to lower cholesterol in familial hypercholesterolaemia).
In secondary prevention, high dose atorvastatin at 80 mg (max dose) is usually prescribed (unlicensed). However, in the presence of significant interactions (see below), this may need reducing.
Contraindications and cautions
Statins should be used with caution in patients with, or at risk, of liver disease (i.e. NAFLD, high alcohol use, raised transaminases).
It is important remember that statins are contraindicated in patients with severe liver disease (i.e. decompensated liver disease, acute liver failure).
Other important cautions are untreated hypothyroidism, history of muscular disorders (see side-effects below), and stroke (hyperacute ischaemic and haemorrhagic). Stroke is a complex area and treatment should be guided by stroke specialists.
Side-effects
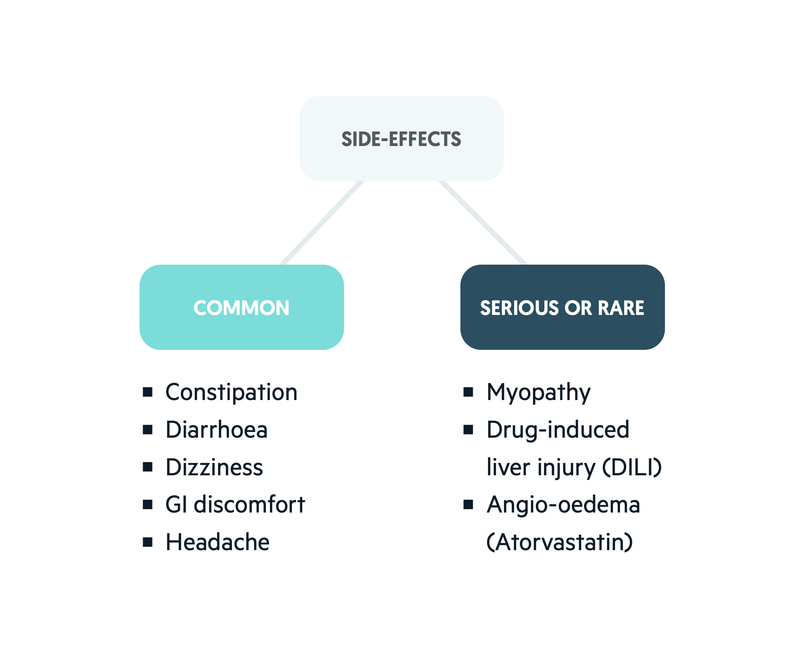
The two important side-effects of statins are drug-induced liver injury (DILI) and myopathy.
Statins are associated with a number of mild side-effects. These range from gastrointestinal disturbances to headaches. Important serious or rare side-effects include DILI, myopathy and neuropathy. There are some statin-specific side-effects like angio-oedema that is associated with atorvastatin.
Drug-induced liver injury
Statin therapy has been associated with development of varying degrees of severity of DILI. Patients with features of hepatotoxicity should have liver function tests checked and NICE recommend routine checks at 3 and 12 months. If transaminases are >3 time upper limit of normal, discontinue statin.
Myopathy
Myopathy describes any type of muscle disease. Statin therapy is associated with a spectrum of skeletal muscle disorders. These disorders include:
- Myalgia (muscle ache, normal creatine kinase)
- Myositis (muscle pain and weakness, inflammation, creatine kinase elevated)
- Rhabdomyolysis (muscle pain and weakness, inflammation, muscle breakdown, creatine kinase markedly elevated).
- Immune-mediate necrotising myopathy (muscle pain and weakness, immune-mediated inflammation, mild-to-moderate CK elevation)
Rhabdomyolysis can be a life-threatening condition associated with acute kidney injury, disseminated intravascular coagulation and multi-organ failure. In patients with muscle cramps and elevated creatine kinase (CK), statins should be discontinued. In mild episodes of myopathy, statins can be reintroduced at a lower dose but expert advice should be sought.
Interactions
Statins have several drug interactions due to their metabolism by the hepatic cytochrome P450 pathway.
Classical interactions include amiodarone and clarithromycin, which are enzyme inhibitors. Co-administration of an enzyme inhibitor leads to an increased risk of myopathy. The BNF should always be consulted for interactions.
Pregnancy and monitoring
Statins are considered teratogenic and should be avoided.
Patients on statin therapy should have blood test monitoring. Baseline lipid profile, CK (if myopathy symptoms), U&Es, LFTs and TFTs should be checked. NICE subsequently recommend LFTs at 3 and 12 months and HbA1c in high-risk patients.
It is important to consider dose adjustment in renal impairment and the BNF or Renal drug handbook should be checked.
Last updated: May 2022
Have comments about these notes? Leave us feedback
