Bronchodilators
Notes
Introduction
Airway resistance occurs as frictional forces oppose the flow of air through the conducting airways. Normal flow is laminar, the flow is ordered and quicker in the centre. As airways divide and become narrow increasingly turbulent flow occurs.
Poiseuille’s equation describes resistance (if flow is laminar) with resistance (R), length (L), radius (r) and viscosity (η). π and 8 are constants:
Resistance (R) = 8 x L x η / π x r4
Bronchomotor tone
Bronchomotor tone controls the ease with which air is conducted through airways. It exhibits a circadian rhythm where tone is greatest in the early morning.
We note from the above equation that a doubling in the radius of an airway (assuming laminar flow) results in a sixteen times reduction in resistance.
Various inhaled stimuli may cause an increase in tone though little is understood about the central control of bronchomotor tone.
Bronchodilators
Bronchodilators act to reduce bronchomotor tone to bring about bronchodilation.
These are symptom relieving treatments that are regularly used in chronic conditions such as asthma and COPD.
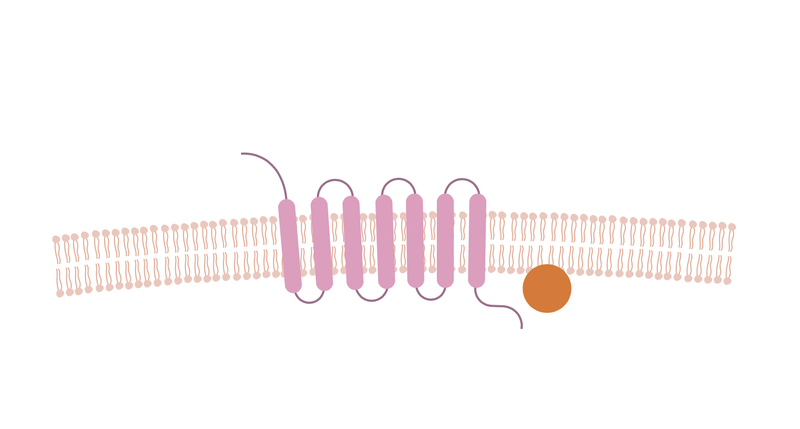
G-protein coupled receptors
G-protein coupled receptors are the largest group of receptors in eukaryotes. They have a seven transmembrane domain i.e. they pass through the cell membrane 7 times.
The classes of bronchodilators discussed in this note have actions that involve G-protein coupled receptors. They are metabotropic receptors - their actions are mediated by a secondary messenger.
Secondary messenger molecules such as cAMP and DAG initiate intracellular signalling pathways. The binding of an agonist to the receptor leads to activation of the G protein and activation of secondary pathways.
Beta-2 agonists
Used in both asthma and COPD this is an important class of bronchodilator. It is utilised in both chronic and acute management of these conditions.
Beta-2 adrenoceptors
Beta-2 adrenoceptors are G-protein coupled receptors found primarily in the lungs. These are key receptors of the sympathetic nervous system that are stimulated by catecholamines such as adrenaline.
Beta-2 adrenoceptors are found throughout the lungs with a particularly high density in the bronchial smooth muscle. Activation of these receptors by the sympathetic nervous system cause bronchodilation through smooth muscle relaxation.
Inhaled agonists
Beta-2 adrenergic agonists are sympathomimetics that activate beta-receptors. These drugs act to relax the airways smooth muscle.
Additional actions include:
- Reduced release of inflammatory mediators from mast cells.
- Increased mucociliary clearance.
Can be short-acting (e.g Salbutamol) or long-acting (e.g Salmeterol):
- Short-acting beta-2 agonists (SABA): The short-acting forms are hydrophilic and as such are quickly metabolised. They have a rapid onset (< 5 minutes) and effects last around 6 hours. They are used as required (PRN). High use indicates inadequately controlled disease.
- Long-acting beta-2 agonists (LABA): The long-acting forms are more lipophilic and effects last for around 12 hours. Used in a regular manner, concordance is often poorer than with SABAs.
Beta-2 agonists show varying degrees of selectivity and may have effects beyond their intended site.
Adverse effects
Many of beta-2 agonists unwanted effects result from its systemic actions:
- Tachycardia: Results from activation of beta-1 (dominant receptor in the heart) and beta-2 adrenoreceptors in the heart. May also cause arrhythmias.
- Tremor: Results from activation of beta-2 adrenoreceptors in skeletal muscle.
- Hypokalaemia: Results from activation of beta-2 adrenoreceptors linked Na/K-ATPase channels leading to increased cellular uptake of potassium. Salbutamol may be used to help treat hyperkalaemia.
Muscarinic antagonists
Used primarily in chronic management of COPD, muscarinic antagonists also play a role in treatment of an acute asthma attack and acute exacerbation of COPD.
Muscarinic receptors
Cholinergic receptors are those that are related to the neurotransmitter acetylcholine. There are two forms, differentiated by their activation with muscarine and nicotine:
- Muscarinic receptors: a metabotropic G-protein coupled receptor activated by muscarine.
- Nicotinic receptors: an ionotropic receptor activated by nicotine
Muscarinic receptors are a key part of the parasympathetic nervous system acting as post-ganglionic receptors activated by acetylcholine.
There are five subtypes. Subtypes M1, M2 and M3 are best characterised. M3 is thought to be the most important in the treatment of chronic airway diseases. Activation of M3 receptors by the parasympathetic nervous system leads to bronchoconstriction.
Inhaled antagonists
Inhaled muscarinic antagonists block the action of muscarinic acetylcholine receptors, they are non-selective. When administered these agents act to relax the airways smooth muscle.
They are primarily of use in the chronic management of COPD but may be used in the treatment of an acute asthma attack.
Can be short-acting (e.g Ipratropium) or long-acting (e.g Tiotropium).
Adverse effects
Typical ‘anti-cholinergic’ effects:
- Dry mouth (xerostomia)
- Urinary retention
- Headache
- Exacerbation of glaucoma (pilocarpine - an agonist of M3 - is used in the treatment of angle-closure glaucoma).
Methylxanthines
Methylxanthines are a nonselective phosphodiesterase (PDE) inhibitor that may be used in the management of COPD and asthma.
They occur naturally and are found in coffee, tea and chocolate. Bronchodilation is one of a number of effects of methylxanthines that contribute to its therapeutic effect. However with the advent of newer bronchodilators, methylxanthines have somewhat fallen from favour.
Theophylline may also be used to treat apnea and bradycardia of prematurity.
Mechanism of action
Two forms are used in clinical practice:
- Theophylline is a naturally occurring methylxanthine.
- Aminophylline is a 2:1 combination of theophylline and ethylenediamine that is more water-soluble. It can also be administered intravenously.
Their action is a result of adenosine receptor antagonism and indirect adrenergic activity.
Methylxanthines have a similar structure to caffeine, they have a wide range of effects including:
- Immunomodulation
- Anti-inflammatory
- Vasodilation
- Bronchodilation
Toxicity
Theophylline and aminophylline have a narrow therapeutic window - with a clinical therapeutic index of 1 to 1.5. The majority of the adverse effects are dose related and are seen more frequently in overdose.
Manifestations of toxicity include:
- Metabolic:
- Hypokalaemia
- Hyperglycaemia
- Cardiovascular:
- Hypotension - PDE3 inhibition of smooth muscle in blood vessels
- Sinus tachycardia
- Tachyarrhythmias
- Gastrointestinal:
- Nausea and vomiting - due to PDE4 inhibition in the vomiting centre
- Diarrhoea
- Neurological:
- Insomnia
- Mood changes
- Seizures
- Muscular:
- Coarse tremor
- Rhabdomyolysis
Inhaler devices
Inhaled devices more accurately target the intended site of action (compared to oral options) allowing for lower therapeutic doses, reduced systemic concentrations and unwanted effects.
There are disadvantages, effective administration via handheld inhalers may require a great deal of patient education. Compliance may be poor and effectiveness in severe disease is reduced.
Metered-dose inhalers
Metered-dose inhalers (MDIs) are aerosol based inhalers, which are the most common delivery device for bronchodilators.
Effective use requires significant patient education to ensure adequate delivery of medication.
Breath-actuated inhalers
Breath-actuated inhalers can deliver a dry powder or aerosol.
Activation is triggered by the patient inhaling. The patient must be able to generate a strong inspiratory flow and as such they are less effective in severe disease.
Volume spacer
Spacer devices are used in conjunction with MDIs. They remove the need for coordination between activation of the inhaler and inhalation.
They are useful for young children and during an acute attack. Increasingly they are being used in the wider population due to poor inhaler technique.
Nebuliser
Nebulisers are typically reserved for acute attacks but may be used at home in those unable to effectively use other devices.
Nebules of liquid are vaporised by either an air jet (jet nebuliser) or vibrations of a piezoelectric crystal (ultrasonic nebuliser).
The vapour is then inhaled via a face mask or mouthpiece. A greater dose is typically required for equivalent effect when compared with a normal inhaler.
Last updated: March 2021
Have comments about these notes? Leave us feedback
